Penn Ostomy Output Program
Project status
Collaborators
Joshua Bleier, MD
Michael Fejka, PA-C
Matthew Ciabattoni, DNP, RN
Lee Leibowitz, MBA
Innovation leads
Opportunity
Dehydration and electrolyte imbalance are the most common drivers of readmissions among patients who have recently undergone an ostomy placement, a surgical procedure that allows fecal waste to pass through the abdomen.
Such readmissions disrupt patient recovery and result in significant care costs.
Intervention
The Penn Ostomy Output Program is an automated text messaging-based solution designed to optimize health outcomes by supporting ostomy patients before surgery and tracking key data after the procedure.
Pre-operatively, patients receive text reminders about how to prepare for their surgery, including instructions for taking antibiotics, bowel prep, and tips for getting their homes ready for their return. After discharge, patients are prompted to report their stool output via text message. If output falls outside of the predetermined limits, the care team receives an alert and adjusts care as needed.
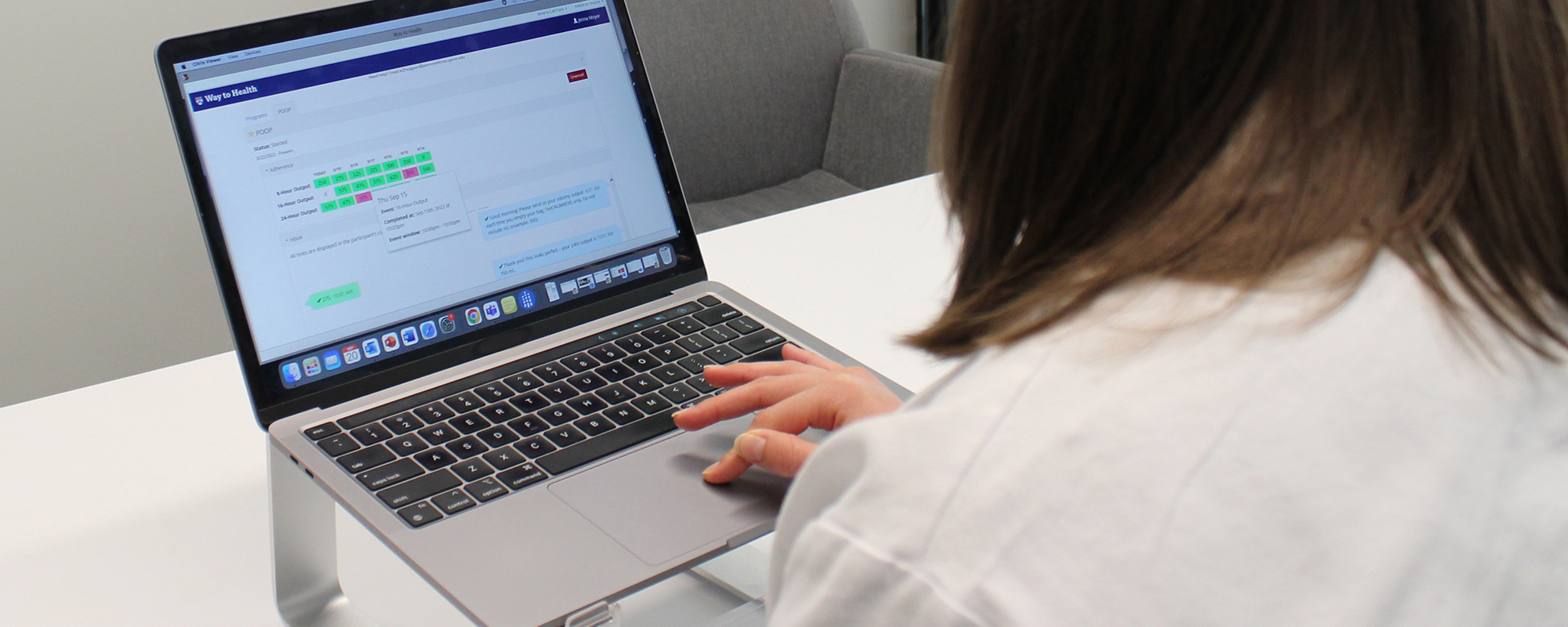
Leveraging the Way to Health platform, the Penn Ostomy Output Program is integrated into the electronic health record for easy enrollment and review of patient output.
Impact
During a yearlong piloting period beginning in August 2020, the program reduced the average ileostomy readmission rate from 23 percent to 16 percent. In addition, nearly two-thirds of the patients enrolled were identified as needing an at-home intervention in the form of medication adjustment, provider phone calls, or home IV fluids to decrease the risk of dehydration. Thanks to these interventions, only two readmissions occurred, neither of which was related to hydration status. The number of prevented readmissions resulted in an estimated cost savings of $100,000.
In October 2021, the Penn Ostomy Output Program scaled to several Penn Medicine hospitals. It is now available to ileostomy patients at the Hospital of the University of Pennsylvania, Penn Presbyterian Medical Center, and Pennsylvania Hospital. Extended to the additional colorectal surgeons at these locations, the program is expected to free up more than 60 patient bed days and save the health system $250,000 annually. Most importantly, it allows surgical teams to continue to support patients through the critical pre-operative and post-discharge periods in ways that were previously unavailable.
Way to Health Specs
Learn more about the platformInnovation Methods
Mini-pilot
Mini-pilot
Mini-pilot
High-fidelity learning can come from low-fidelity deployment.
Mini-pilots will allow you to learn by doing, usually by deploying a fake back end. You might try a new intervention with ten patients over two days in one clinic, using manual processes for what might ultimately be automated.
Running a "pop-up" novel clinic or offering a different path to a handful of patients will enable you to learn what works and what doesn't more quickly. And, limiting the scope can help you gain buy-in from stakeholders to get your solution out into the world with users and test safely.
Mini-pilot
Due to a reduction in surgeries during the COVID-19 pandemic, we conducted initial quality assurance and testing with staff members and providers. We learned that the timing of provider alerts needed to be adjusted for greater response efficiency and that additional patient encouragement would be necessary for real-time output monitoring. Once surgeries restarted, we began a mini-pilot with two ileostomy patients over two weeks. Patient questions and feedback led us to include automated calculation responses that eliminated the need for patients to complete manual calculations. We also implemented a more simplified output chart to enable more straightforward provider analysis.